Age
18 - None
Check your eligibility now & get in touch with a study center
CHECK ELIGIBILITYBackground: Thiamine deficiency (TD) causes a variety of thiamine deficiency disorders (TDDs) such as neuropsychiatric disturbances, polyneuropathy, ataxia, weakness and falling, and non-ischemic heart failure. Left untreated, TD can be associated with poor quality of life, loss of independence, and inability to complete activities of daily living. The prevalence of TD in non-alcohol using hospitalized Veterans is not known but is probably much higher than the general population. Loss of functional ability leads to increased need for rehabilitation.
The objective of this proposal is to measure the prevalence of TDDs in Veterans who do not use excess alcohol who are ill enough to require hospitalization, determine if inflammation increases the risk of developing TD, and determine the optimal cutoff points for two biomarkers of TD to diagnose of TDDs. The central hypothesis is that TD prevalence is as high as 25% in hospitalized non-alcoholic Veterans, far greater than the historically reported prevalence of 3% or less, and that TDD's occur in the "low normal" range of current cutoff values for available thiamine bioassays. A secondary hypothesis is that inflammatory conditions, which are known to cause cachexia and malnutrition, put hospitalized Veterans at increased risk as they often present with acute inflammatory conditions. The rationale underlying this proposal is that hospital practitioners currently underdiagnose and undertreat TDDs which leads to continued morbidity and loss of function. If our hypothesis is correct that the prevalence is as high as 25%, this knowledge will increase awareness of the problem and lead practitioners to diagnose and treat them more often. In addition, clarifying the "abnormally low" biomarker cutoff levels by measuring them in Veterans with TDDs is very important as the current "normal" ranges were determined in healthy volunteers. The central hypothesis will be tested by pursuing three specific aims: 1) determine the prevalence of TD, as defined by whole blood and plasma thiamine levels together with symptom responsive disease in consecutively hospitalized medicine patients who do not use excessive alcohol; 2) define TDDs as cases with low or "low normal" thiamine levels and symptoms that improve with thiamine replenishment; 3) determine if acute and chronic inflammatory conditions with elevated biomarkers of inflammation increase the risk of developing TDD. We expect to find the prevalence of TD is closer to 25% and that the low end of "normal" biomarker levels as published by reference laboratories is too low, missing a percentage of TDDs.
Research design: To accomplish these aims, we will utilize a prospective cohort study design to determine the prevalence of TD in consecutively hospitalized non-alcoholic medicine patients, as defined by low or "low normal" thiamine biomarker levels and thiamine responsive symptoms. Nested within this we will conduct an open label treatment study with those exhibiting symptoms and define TDDs as cases with low or "low normal" thiamine levels and symptoms of TD that improve with thiamine administration. Lastly, utilizing a nested case control study design with cases being those with a TDD and controls being asymptomatic Veterans with normal biomarkers, determine if acute and chronic inflammatory conditions with elevated biomarkers of inflammation increase the risk of developing TDDs.
You can use content blocks to arrange your articles, large texts, instructions. Combine these blocks with media blocks to add illustrations and video tutorials. You can use various content blocks to work with your text. Add quotations, lists, buttons. Select your text to change its formatting or add links. You can use various content blocks to work with your text. Add quotations, lists, buttons. Select your text to change its formatting or add links.
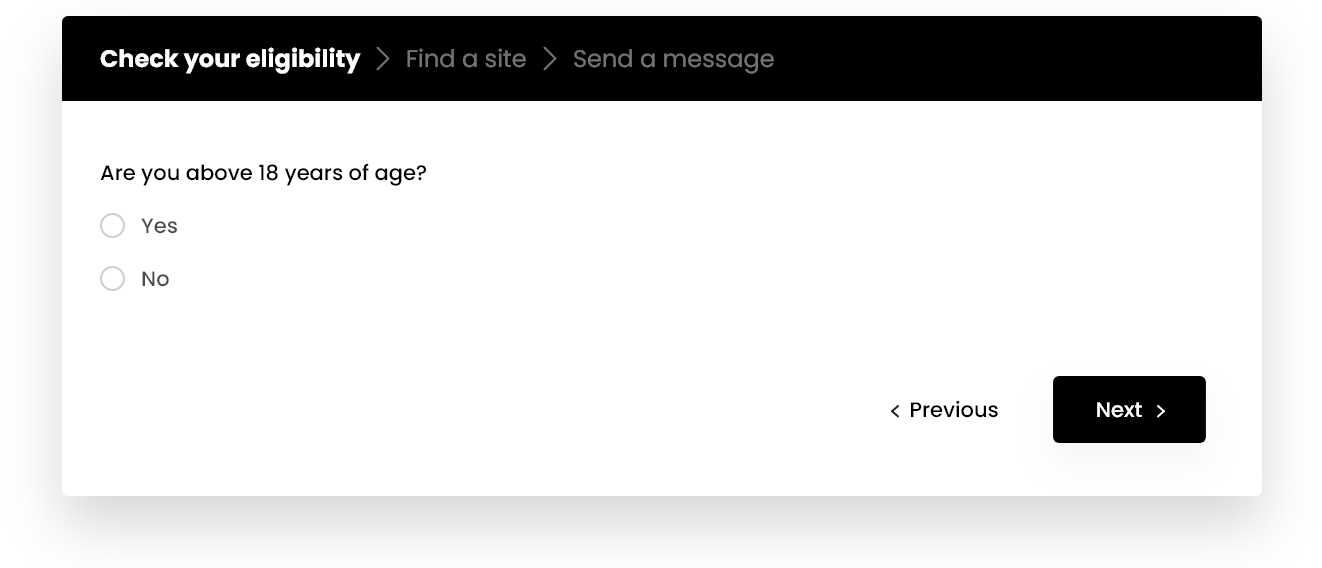
Take up this questionnaire to help us determine if you have symptoms that are common to this clinical study. If you have the common symptoms, you may be eligible to take part in the study.
18 - None
Both
NCT05480943
-1
Recruiting Now
Thiamine Deficiency
A short sentence to introduce what to expect in the about condition section
Learn moreA short sentence to introduce what to expect in the about condition section
Learn moreA short sentence to introduce what to expect in the about condition section
Learn moreYou would receive etanercept (Enbrel) twice a week for 12 weeks and then once a week for 12 weeks. Etanercept, as well as study related medical care, is provided at no cost.
Study participation involves approximately 8 visits to your local study center over 6 to 7 months.
There would also be a follow-up telephone call 30days after completing the study. No visits are required after participation is complete.